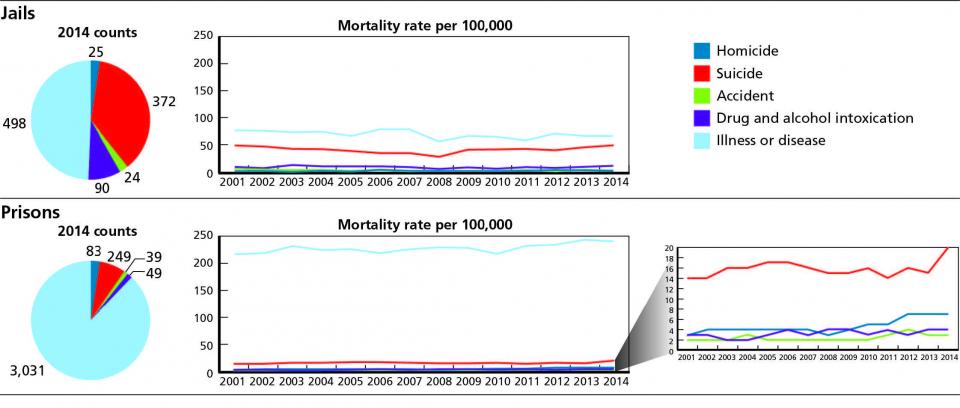
For most people, the notion that our prisons and jails are fortified against escape is sufficient. The general public knows relatively little of what goes on behind the walls, in terms of the health and welfare of incarcerated persons. Recently, however, in light of a rise in deaths attributed to suicide and drug and alcohol intoxication, renewed attention has focused on the issue of mortality of incarcerated persons (Figure 1).
RAND Corporation and the University of Denver (DU) analyzed insights from a working group of experts with practical expertise in and knowledge of mortality trends. To reduce mortality, the study, sponsored by the National Institute of Justice (NIJ), identified a series of systemic needs grouped under the following six themes:
- Supporting evidence-based practices and national standards for the health care of incarcerated persons.
- Improving capacity to provide medical and mental health care.
- Improving organizational culture and operations.
- Strengthening coordination and continuity of care.
- Leveraging pharmacological advances.
- Strengthening analysis and
- use of data.
The working group’s findings, discussed below, suggest that reductions in mortality can be achieved through organizational change supporting emphasis on care objectives equal to the emphasis on custody and control objectives, adherence to best practices and adequate resources to provide quality care to individuals before, during and after incarceration.
Nature and scope of the problem
Maintaining the health and safety of incarcerated persons — and ultimately reducing the mortality rate — is a complex and challenging task, albeit one that should be at the core of the correctional mission. Prisons and jails have a constitutional obligation to care for the incarcerated population and, ultimately, most forms of mortality within correctional facilities are preventable, to varying degrees, with the proper interventions. Many incarcerated persons enter facilities in poor health. They disproportionately suffer from mental illness, disease and addiction; many are prone to violence. The conditions of confinement can be detrimental to overall health and safety in a variety of ways and can exacerbate certain preexisting conditions. Studies have established that these findings are consistent.[1]
Once consequences of the growth in incarceration rates has been the confinement of greater numbers of generally unhealthy individuals for longer periods of time. That, coupled with rising health costs, generally represents a significant taxpayer burden. Although there is great variance in the quality of care provided by facilities across the country, in general these factors, combined with resource constraints at all levels of government, make it difficult to maintain appropriate standards of care for incarcerated persons.
Study purpose
The joint RAND-DU study on mortality, “Caring for Those in Custody: Identifying High Priority Needs to Reduce Mortality in Correctional Facilities,” is part of a multiyear research effort, the Priority Criminal Justice Needs Initiative, to identify innovations in technology, policy and practice that benefits the criminal justice sector.[2] In response to a recent increase in mortality rates, the study aimed at producing a better understanding of factors contributing to mortality and identifying key needs associated with improving outcomes. The results also help inform NIJ’s research agenda moving forward and, along with future research, will help guide policy-makers and facility leaders on addressing care needs.
Methodology
The research team assembled a group of 16 individuals with expertise and knowledge of corrections and correctional health care to participate in a two-day workshop. Care was taken to include participants with experience and expertise in jails or prisons (or both), recognizing that each setting is unique.
One noteworthy difference is the higher overall incidence of suicide in jails than in prisons, attributable, in part, to the fact that those entering jail, as opposed to prison, often face an immediate crisis situation as they experience penal confinement for the first time. Before the workshop, in order to focus discussion, participants were given a copy of the Bureau of Justice Statistics’ (BJS) most recent report on deaths in correctional facilities, “Mortality in Local Jails and State Prisons, 2000-2013.” This report provides national and state-level data on the number and rate of deaths of incarcerated individuals across a number of variables, including cause of death, type of facility, state and characteristics of incarcerated individuals — such as age, sex and race — over a 14-year period.
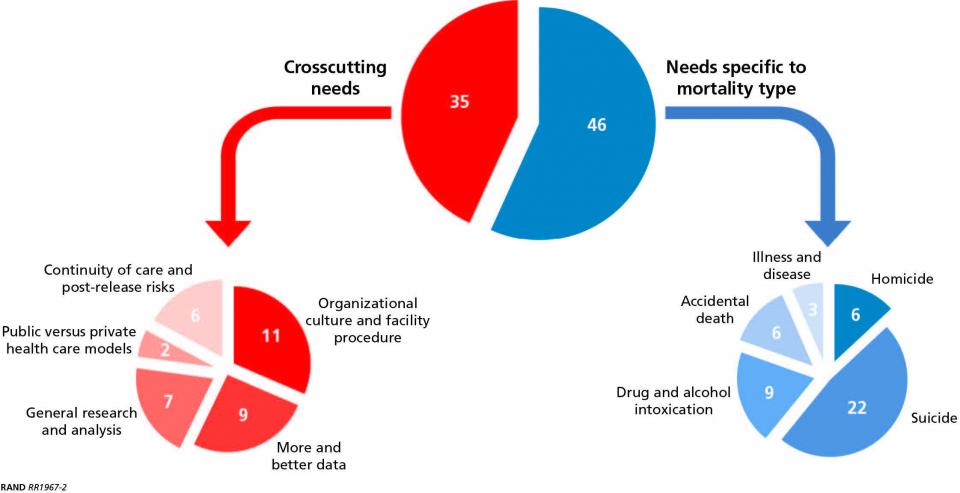
During the two-day workshop, participants were divided into two breakout groups (prisons and jails). Researchers conducted highly-structured exercises with each group in order to elicit information about the most pressing problems related to mortality and to assess how the problems could be addressed. Discussions focused on each of the five major mortality types identified in the BJS report (illness or disease, homicide, suicide, drug or alcohol intoxication and accidental death), as well as general or more cross-cutting issues that were not specific to any particular type of mortality. From these discussions, the research team identified a set of discrete needs. This process yielded a total of 81 needs between the two breakout groups (Figure 2).
To provide structure to this large set of identified needs, participants ranked each need in terms of expected benefit (relative importance of meeting that need) and probability of success of actually meeting that need. These ratings were multiplied to produce an expected value score, and that score was used to group the needs into top, medium and low tiers. In the final analysis, 15 of the 81 identified needs were ranked in the top tier.
The following key themes emerged:
Supporting evidence-based practices and national standards
At various times during the workshop, the group discussed the importance of best practices and established standards with respect to general health care, agreeing that compliance is key to better outcomes. Much of the focus was on suicide prevention, with an emphasis on risk assessment. Reflecting the group’s view that the use of benchmarks is uneven across the country, four top-tier needs emerged within this theme. Overall, there is a need to more effectively promulgate best practices as they evolve. On the research side, the working group identified a need to better understand current levels of adherence to standards and best practices, as well as barriers to implementation, and to identify strategies to incentivize wider adoption.
Improving capacity to provide medical and mental health care
Three of the top-tier needs were related to deficiencies in the capacity to provide care (Figure 3). As correctional facilities operate in a resource-challenged environment, the needs of the incarcerated population are often not fully met. Given the substantial mental health needs and increased risk of suicide among this population, there is a need for an improved level of mental health care in correctional facilities that is comparable to community-level care, the group concluded. This includes strategies that provide incentives for mental health professionals to work in the correctional environment. On the medical side, an increase in the capacity to detect acute chronic conditions and provide an intermediate level of care on-site would reduce mortality, particularly in facilities located in remote areas. Addressing this need is of particular importance.
Improving organizational culture and operations
The importance of strong collaboration between security and medical staff is critical, the group concluded. This theme extends to positioning medical authorities at leadership levels of the organization to ensure that health care objectives are given adequate weight. Other needs include the development of strategies to overcome inherent conflicts between security and health care objectives that negatively affect care delivery. Further, there is a need to break existing cultural barriers that prevent staff from providing positive input outside of their functional areas. Facilities can benefit from the use of cross-disciplinary teams and other collaborative approaches that generate innovative ways to reduce mortality, the experts advised.
Strengthening coordination and continuity of care
There are shortfalls associated with the fragmented nature of the public and correctional health systems, the group observed. Individuals with long-term involvement with the justice system routinely flow from the community to jail, to prison, and then back to the community. To improve health outcomes, there is a need for stronger partnerships and “warm handoffs” between the various organizations that provide care. (Warm handoffs between providers are conducted in person, in the presence of the patient and if possible with family present.) Included in this theme are needs for systems, standards and methods to facilitate sharing of pertinent health data between correctional entities.
Leveraging pharmacological advances
Reflecting on the impact of the national opioid epidemic, two top-tier needs called for the expansion of the use of pharmacological approaches to treating those with substance abuse disorders. Because they are at an increased risk of death, facilities should make medication-assisted treatment available to them and provide staff with greater access to drug overdose countermeasures.
Strengthening analysis and the use of data
One final top-tier need identified by the working group fell within this theme: Beyond a call for increased granularity and increased accuracy of mortality statistics mentioned in other, lower ranked needs, there is a need for better data collection and analyses of “near-misses” (i.e., incidents that did not ultimately result in death, but easily could have).
Conclusion
The majority of the needs identified in the RAND-DU report on responses to mortality of incarcerated individuals are not new. Indeed, several closely mirror previous recommendations made by national correctional health care organizations.[3] This implies a consensus on at least a subset of the requirements to improve correctional health outcomes, which lead to reductions in mortality. As with many other systemic problems in the corrections environment, the gap between needs and solutions appears to be a function of prioritization, occurring on two levels. The experts who convened for this working group agree that correctional facilities share the common objectives of care, custody and control of the incarcerated population. However, these objectives are generally not equally emphasized, according to the working group. Caring for the incarcerated is often subordinate to the need for containment and security. Thus, in the group’s view, organizational change is needed to achieve better mortality outcomes.
It must be recognized that preventable deaths represent a system failure, according to the working group. Custody and medical staff must work collaboratively to identify and mitigate risks on an ongoing basis. Effective correctional leadership is key in establishing a culture that effectively balances a facility’s security requirements with the health and safety needs of the incarcerated population, the experts agreed. Leaders must instill in their staff the message that everyone is responsible for the health and safety of the incarcerated population.
A the societal level, transformational change can only be achieved through the dedication of adequate medical and mental health resources in both institutions and communities, the working group concluded. Individuals who come into contact with the justice system are at risk for poor health outcomes and, as noted, many convicted and sentenced persons arrive at correctional facilities in poor health. That reality reflects inadequate access to care and treatment in the community.
With respect to mental health and substance abuse services, the working group concluded the capacity for care in the community must be greatly expanded. Addressing these needs at the earliest opportunity can not only enhance the health of incarcerated persons while reducing mortality rates among the incarcerated, but research indicates it can also reduce crime and ultimately incarceration.[4] Facilities need to expand their care capacity as well, the experts concluded. The public needs to be educated on the fact that a majority of those incarcerated will be released into the community at some point, and their illnesses, diseases and addictions will return with them if they are not detected and effectively treated during incarceration. Investments in correctional health care not only serve to meet constitutional obligations regarding the treatment of persons in custody, they reduce mortality. Moreover, healthier individuals will return to their communities upon release.
Finally, the expert working group in the RAND-DU study concluded that the capacity for mental health and substance abuse services dedicated for the formerly incarcerated should be greatly expanded. The period of transition to the community can be extremely difficult. During the two weeks following release, formerly incarcerated persons are 13 times more likely to die than those in the general population.[5] Systemic changes are required to facilitate warm hand-offs between facilities and community-based providers, in the experts’ view.
Greater investments in health care for individuals before, during and after incarceration can not only reduce mortality, but can also reduce criminality in a cost-effective manner. The needs identified in this report represent a strong and diverse agenda that can serve as a foundation for transformational change, given the social and political will to pursue this direction. View the full report.
Sidebar: Top Tier Needs
- National standards governing medical screening are not being universally adopted and used by facilities. Research is needed to assess the level of compliance with these standards and to quantify the impact that compliance has on morbidity and mortality. Further, financial and other support is required for facilities that wish to meet these standards.
- Because some types of mortality are relatively rare, more granular data on “near misses” should be collected and analyzed. These data are critically important to better understanding incidents and developing prevention strategies.
- To better serve the health care needs of the incarcerated, facilities need greater capacity to both detect the acute chronic conditions and to respond with intermediate level of care.
- To help ensure that health care issues receive the appropriate level of attention within an agency or facility, organizational structures should designate authority and autonomy to medical officials.
- The inherent conflicts between security and medical objectives can make it challenging to deliver quality health care
- on a day-to-day basis. There is a need for collaborative approaches to overcome these obstacles.
- The prevailing correctional culture tends to encourage security and medical staff to focus only on their individual areas, which inhibits innovative approaches to reduce mortality. Strategies are needed that promote greater cooperation and collaboration in processes such as death reviews.
- To help prevent death of incarcerated individuals due to drug overdose, staff need greater access to countermeasures, such as naloxone, as well as supporting policies, procedures and standards to guide their use.
- Corrections agencies need to expand the use of medication-assisted treatment, a proven intervention in community-level care, in support of desistence from drugs.
- Evidence-based suicide prevention strategies, including the use of risk assessment instruments validated in the correctional environment, are not uniformly implemented across the country. There is a need to assess the extent of implementation, identify barriers and develop strategies to incentivize and support implementation.
- Because suicide risk is dynamic rather than static, processes are needed to support rescreening at regular intervals and after key events in the incarcerated person’s life.
- Suicide risk assessment is not always reliable. There is a need to promulgate best practices, specifically related to the use of skilled screeners in private environments more conducive to sensitive discussion.
- With respect to mental health services, there is a wide discrepancy between the community level of care and that which is provided in correctional facilities. There is a need for cost-benefit analyses of providing community-level of care in correctional facilities.
- Many facilities suffer from a shortage of mental health treatment providers. There is a need for creative funding solutions or other incentives to support the required capacity.
- There is a lack of coordination between providers of health care services in facilities and those in the general community. This has a negative impact on the health care of individuals, particularly those who are frequently incarcerated for relatively short periods of time. There is a need to incentivize partnerships between providers to improve health
- care outcomes.
- As individuals move from jails to prisons, pertinent health care information is not consistently shared. Systems, standards and methodologies are needed for facility health care information exchange between correctional entities. Education is also needed to clarify common misinterpretations of HIPAA regulations.
About the Author
Joe Russo is the corrections technology lead at the Justice Technology Information Center, an NIJ program funded through a grant to Leidos Innovations Corporation. Russo is a co-author of the report that is the subject of this article.