Before x-ray technology, broken bones and bullet location were detected by “physical examination and a doctor’s best guess.”[1] There was no way for a physician to see into the human body without incising it. Then, on November 8, 1895, German physics professor Wilhelm Conrad Röntgen made an astonishing discovery that would forever change diagnostic medicine. While working with high-voltage electricity, cathode rays, and gases at low pressure, he found that “x-rays” could penetrate most solid objects.[2] For the first time, physicians were able to noninvasively see the human anatomy. Interestingly, Röntgen’s first image was the internal structure of his wife's hand (see exhibit 1).
In 1895, John Macintyre established the world’s first radiology department at Glasgow Royal Infirmary in Scotland. Early successes included producing the first images of a renal stone. That same year, Walter Bradford Cannon, an American physiologist, used x-rays to follow food passing through an animal’s digestive system.[3] In 1896, physicians began to use x-rays for medicolegal purposes, most often for gunshot cases, tumor identification, and dental examinations.[4] Over the next 100 years, x-ray technology continued to advance, and imaging helped supplement the scalpel. By the 1980s, Europe saw the early use of virtual or digital autopsies, followed by three-dimensional, multiplanar scans in the early 1990s (see exhibit 2).[5]
Today, using computed tomography (CT) scanning technology — or computerized x-ray imaging[6] — to augment autopsies is fairly commonplace in Europe, Japan, and Australia. In the United States, however, the practice is not as routine, for reasons we will discuss throughout the article.[7] In some situations, the use of advanced imaging technologies, such as CT, prior to or in place of a traditional autopsy would be advantageous and could offer solutions to some challenges faced by the medicolegal community, such as limited resources or conditions or circumstances that make the cause of death not easily diagnosed through a traditional (gross anatomy) autopsy. Through research and international partnerships, NIJ is working to inform the community of potential benefits and advance this resource to medical examiners and coroners nationwide.
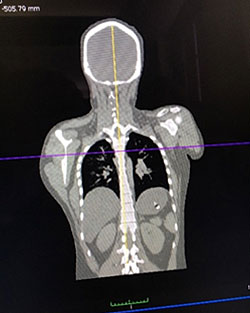
The first image shows a three-dimensional rendering of a torso showing hip fractures. The second image is a computed tomography (CT) scan of a torso on a coronal plane. Both images were viewed through a program called OsiriX.
Many U.S. offices have started to embrace Lodox imaging technology, which is a high-quality, low-dose, digital x-ray that can scan an entire body.[8] Lodox was invented in South Africa to see if those who work in diamond mines had swallowed diamonds from the mines.[9] Over time, U.S. trauma centers and medical examiner offices have incorporated the use of Lodox, which is fast, less expensive than traditional x-rays, and has specific benefits. For example, it can detect specific medical occurrences or features, such as pneumothoraces and bone fractures near the skin’s surface, and metal objects such as projectiles and implants. Although Lodox would not replace CT, it is a gateway to new technology. CT technology allows physicians to better visualize areas that are harder to dissect, visualize vessels (including stenosis, occlusion, and ruptures) and stab wounds using radio-opaque dyes, and estimate the volume of hemorrhages.
When an unattended or suspicious death comes to a morgue in the United States, a forensic pathologist — a physician who works as a medical examiner and performs autopsies to determine the cause of death — typically conducts a traditional autopsy. Although we often emphasize the criminal justice or legal aspects of medicolegal investigations, we sometimes forget that medical examiners are physicians who practice medicine; their experience, knowledge, and the tools at their disposal are essential in determining the cause and manner of death.
Meeting the Needs of the Community
About 2.6 million people die each year in the United States; approximately 500,000 of them receive post-mortem examinations.[10] Currently, the nation has a shortage of board-certified forensic pathologists. Projections suggest that 1,000 board-certified forensic pathologists are needed to provide adequate coverage in the United States; however, there are only an estimated 500 full-time forensic pathologists.[11] There is a tremendous need to develop and implement advanced methods that could not only enhance autopsies diagnostically but also help combat this shortfall and reduce workloads.[12]
For example, burn victims and motor vehicle fatalities can sometimes present with injuries that are difficult to discern due to the condition of the body. Imaging technology, such as CT, could help pathologists evaluate these cases more quickly without needing to complete a time-consuming gross autopsy. A CT radiograph might offer the pathologist a clear and apparent cause of death without conducting a full autopsy. Another significant advantage to using imaging technology is that the pathologist never loses the ability to delve further if a case requires additional investigation — the use of imaging does not impede the option of going back to a traditional autopsy to supplement findings.
The question of who examines and evaluates CT radiographs can present a potential challenge, as pathologists currently do not perform these duties. However, this is not an unmanageable concern. First, medical examiners’ and coroners’ offices can supplement their staff with radiologists, who can triage and manage a portion of their office’s caseload. Pathologists can also be trained to review radiographs, which may assuage the need to hire additional staff. Some of the offices’ cases might then be resolved quickly through imaging, thus realizing significant time savings. More importantly, because forensic pathologists are experienced in examining the deceased, they are in a better position to interpret the nuances of post-mortem change, such as interpreting what is an actual injury versus what may be imaging artifacts or changes due to decomposition or insect predation; hospital pathologists do not have such experience or exposure.[13]
Additionally, CT may allow medical examiners to better meet the needs of families. Some groups may object to a traditional autopsy because of religious or cultural considerations (e.g., those who are Jewish, Muslim, and Native American).[14], [15] In these circumstances, CT offers a noninvasive alternative that will avoid distressing a family further during a difficult time. Some cultures also have traditions regarding the expediency of burial timeframes; imaging would allow the pathologist to resolve a case within such customary requests. Further, from a medicolegal perspective, imaging might be the only diagnostic tool available to the pathologist to determine the cause of death, as some state laws prevent a medical examiner from performing an autopsy over a family’s objection.[16]
Imaging might also enable nationwide collaboration through telemedicine and technical reviews, especially in regions of the country that lack medical examiner services. In addition, if a case moves to the prosecutorial stage, use of CT-type images as courtroom exhibits may be more palatable to judges and juries than gross anatomy photos showing massive or severe injury.
Making imaging technology available to pathologists as common practice will take effort and persistence. The use of advanced imaging techniques offers agencies a way to reduce the number of gross autopsies needed, address the shortage of forensic pathologists, decrease the number of biohazard exposures, honor our nation’s diverse cultural traditions and, most importantly, increase the amount of diagnostic information that is captured and retained electronically. Unfortunately, the use of CT is not commonplace in much of the United States, for many reasons, including the cost and maintenance of CT equipment, the lack of temperature-controlled facilities with adequate structural integrity, lack of access to and availability of experienced individuals who are able to read and interpret CT images, and the need for additional research. These challenges are not insurmountable and the benefits far outweigh the burdens; it is important to identify solutions and find a way to achieve practical application and cost-effective implementation in this country.
Old Technology, New Practice
Some U.S. agencies have made great strides in bringing CT technology to their medicolegal community. For example, four agencies in this country have in-house CT scanning equipment. The Armed Forces Medical Examiner’s Office (AFMEO), located in Dover, Delaware, focuses solely on U.S. servicemen and servicewomen. AFMEO scans every decedent who comes through its morgue and is using fellowships to advance training in this area. The Chief Medical Examiner’s Office in Maryland also has a CT scanner, which it uses in about half of its cases each year; a radiologist works with the medical examiner and provides consultation.[17] The New Mexico Office of the Medical Investigator (NMOMI) and the Los Angeles County Coroner/Medical Examiner also have in-house CT scanning equipment that has been very effective in daily practice.[18]
Creating Global Partnerships
NIJ is working to advance imaging technology for medical examiners and coroners nationwide. For example, NIJ currently supports cutting-edge research[19] being conducted at the University of New Mexico Health Sciences Center[20] and hosted a technology transition workshop[21] at NMOMI through its Forensic Technology Center of Excellence.[22]
In collaboration with the Netherlands Forensic Institute (NFI), NIJ created and shaped the International Forensic Radiology Research Summit (IFRRS), an international working group looking to establish a research agenda of high-priority needs concerning advanced imaging technologies for forensic pathology applications. In 2011, NIJ entered into a memorandum of understanding with NFI and the Netherlands Organisation for Scientific Research, Chemical and Physical Sciences Division, to advance cooperation and information sharing for the development of effective solutions and priorities that will improve forensic science and criminal justice research. NIJ and NFI identified a mutual need focusing on research and practice in forensic radiology. In 2015, NIJ, NFI, and leadership from the Joint Congress of the International Society for Forensic Radiology and Imaging (ISFRI) and the International Association of Forensic Radiographers (IAFR) began preparations to convene a working group of professionals in forensic radiology to produce a road map to address gaps, challenges, and research needs in the field. On May 10-11, 2016, the IFRRS was held at the Academic Medical Center in Amsterdam, in conjunction with the ISFRI and the IAFR.
Research-Guided Solutions
The IFRRS, spearheaded by NIJ and NFI and with the support of the ISFRI and the IAFR, brought together 40 leading researchers, practicing medical and forensic professionals, and government employees from 11 countries[23] to build research partnerships, encourage collaborations in the global community of forensic radiology, address challenges, and identify possible solutions for the implementation of advanced imaging technologies in medicolegal practice. During the two-day meeting, Dr. Gregory G. Davis, chief coroner/medical examiner in Jefferson County, Alabama, facilitated a discussion with the expert working group that focused on developments and challenges in implementing forensic radiology techniques and research priorities. The expertise and leadership offered by the working group produced a series of priority areas, including but not limited to big data and statistics, age estimation and reconstruction, multimodal imaging, and visualization and presentation.[24]
Using big data to enhance research
Many countries have a common desire to perform research. However, not all countries have the same access to relevant data, as the prevalence of crime affecting their communities may not be equal in volume. The working group noted that an agency’s caseload might be insufficient to conduct a statistically relevant study and recommended that an international clinical and forensic reference database be created for medicolegal research purposes.[25] For instance, many countries do not have the same prevalence of gun violence as that found in the United States, and a collaboration with the United States might provide a larger data set that could potentially offer results with greater statistical significance.
Additional research is needed to collect data and solidify the effectiveness of imaging within certain populations, such as pediatric and elder abuse cases. Research would also help propel the practice forward through the development of machine-driven, automated image assessments, which, up until now, have demonstrated poor results. Big data sets might also provide a robust evaluation pool to assess the skills of radiologists compared to other experts, which might lead to better training protocols to improve techniques and procedures when dealing with decedents.
Profile characteristic estimation and scene reconstruction
The working group also discussed age estimation and reconstruction. Population frequencies and variation, extrapolated from biological profiles, are used to better estimate age, sex, stature, and ancestry. Additional research is needed to further support the data and strengthen biological profile assessment.
Innovative use of technology would be valuable to identify victims of disasters, particularly in situations in which fingerprint collection is unavailable or DNA collection is too risky due to scene hazards. For instance, mobile scanning technology could capture images of body position to preserve the orientation of injuries; the United Kingdom has been using portable scanners for several years.[26] Clinical radiology and imaging used in diagnostics are also well established; however, the working group noted that further research is needed when applying these techniques to post-mortem investigations.
Multimodal imaging
Combining traditional methods with novel techniques — referred to as “multimodal approaches” — can provide pathologists with a more detailed picture. For example, the combination of magnetic resonance imaging (MRI) and near-infrared optical spectroscopy has been used successfully to identify malignant and benign breast tumors.[27] CT/MRI data that date injuries in living patients over time could be compared with scans of the deceased to more accurately identify and date ante- and post-mortem injuries and identify changes (e.g., those caused by decomposition). Although MRI and near-infrared optical spectroscopy are not commonly used by medical examiners, opportunities for growth and research into these new areas should be considered.
Demonstrative aids and presentation in court
Using visual aids to present evidence in court is incredibly important. In homicide cases, the expert opinions and exhibits provided by the medical examiner are invaluable. More robust research is needed that supports how to better and more reliably portray visual aids and how to properly present to the jury what scenarios align with the evidence. For example, animations are based on theory rather than documentation, and it is difficult to get animations admitted into court. In contrast, radiological scans are already used in court to depict injury, eliminating the need to show inflammatory photographs to the jury. However, currently no research addresses quantifying the utility of demonstrative aids and illustrations used in court; evidence-based data of this type would be extremely beneficial to the criminal justice system.
Looking Ahead
Although there are challenges in transitioning advanced imaging technologies (such as CT) into medical examiner and coroner offices, continued research will provide a better understanding of the applications and limitations of advanced imaging for forensic pathology. The benefits could likely offset many challenges faced by forensic pathologists (such as cultural or religious objections), alleviate the volume of cases, and allay efforts to complete all cases through gross autopsy. Furthermore, advanced imaging technologies in forensic pathology could improve courtroom displays, facilitate telemedicine, and provide a permanent objective data archive.[28] Imaging could be used as a complementary tool. Other technologies, such as Lodox, could also be considered — not in place of CT, but to augment medicolegal practice beyond traditional x-rays. Forensic pathologists need access to investigative tools that will ensure decedents are given equal care to the living and that medical examiners are providing robust information to the criminal justice community.
Continued collaborations, information sharing, technology transition, and support of a robust research agenda in advanced imaging for forensic pathology will serve to improve medicolegal death investigations in the United States.
For More Information
Learn more about NIJ's work related to forensic pathology.
About This Article
This article was published as part of NIJ Journal issue number 279, published April 2018.
This article discusses the following grants:
- “Investigation of the Impact of Body Temperature and Post-Mortem Interval on Magnetic Resonance Imaging (MRI) of Unfixed Tissue,” grant number 2012-DN-BX-K019
- “Investigation of Post-Mortem Magnetic Resonance Imaging for the Detection of Intraneural Hemorrhage,” grant number 2013-DN-BX-K004
- “Evaluation of the Routine Use of CT Scanning to Supplant or Supplement Autopsy in a High-Volume Medical Examiner's Office,” grant number 2016-DN-BX-K002
- “Improving and Evaluating Computed Tomography and Magnetic Resonance Imaging in the Investigation of Fatalities Involving Suspected Head Trauma,” grant number 2016-DN-BX-0173
- “Facilitating Forensic Research in Multiple Fields Using a Unique Computed Tomography Dataset,” grant number 2016-DN-BX-0144